Gallbladder and gallstones Kouawai me kōhatu kouawai
Your gallbladder is a small organ that sits near your liver within your tummy (abdomen). It stores bile, a fluid made by your liver. Bile is released from your gallbladder into your intestine (bowel) to help digest the fats in your diet. Sometimes stones can form in the gallbladder. Gallstones are common.
Causes of gallstones
Gallstones are more common in women than men and occur more often as you get older.
They form in the gallbladder from bile salts, fat (mainly cholesterol) and calcium. There can be a single large stone or many small stones.
There is no one cause of gallstones but there are a several risk factors that make you more likely to get them, including:
- age
- family history (close whānau who have had gallstones)
- being overweight or having rapid weight loss (for example, after stomach reduction surgery)
- diabetes
- pregnancy
- oral contraceptives.
Symptoms of gallstones
Most people have no symptoms, and the stones are often only found on a scan arranged for other reasons.
Gallstones cause a problem when they block the exit to the gallbladder. This causes a pain called biliary colic — the most common problem caused by gallstones.
Biliary colic
Biliary colic is a pain that usually happens after a meal, especially a fatty meal.
It is usually a moderately severe pain in the upper right-hand side of your tummy. The pain may go through or around to your back. It can come and go in intensity and last for several hours. You may feel bloated and sick (nauseated) or it may make you throw up (vomit).
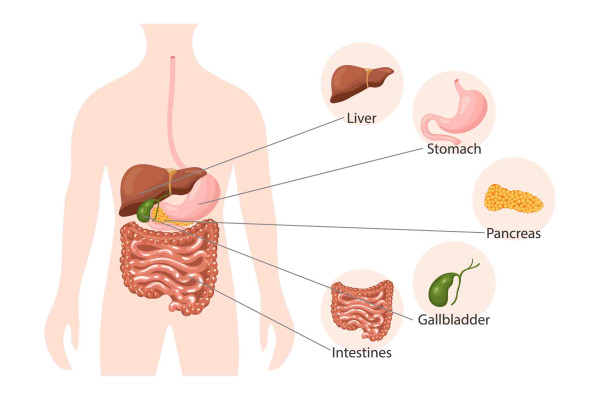
Anatomy of the digestive system
Diagnosing gallstones
If your healthcare provider suspects you may have gallstones, they will refer you for an ultrasound scan.
This scan will show the stones in your gallbladder, if you have them. The scan may also show any stone in your main bile drainage pipe (common bile duct).
It is common to find out you have gallstones when you have an abdominal ultrasound or CT scan for another reason.
If you end up in hospital and initial investigations suggest there may be a blocked bile duct, you may have an investigation called an MRCP (magnetic resonance cholangiopancreatography). This is another way to image your gallbladder and bile ducts.
Treating gallstones
If you have no symptoms from your gallstones, you do not need any treatment. Your healthcare provider may suggest you follow a diet that reduces your chances of forming more gallstones.
If you develop biliary colic, your healthcare provider will give you pain relief medicine. Occasionally, the pain can be severe, and you will need hospital treatment.
If you develop cholecystitis or cholangitis, you will need to be treated in hospital with antibiotics and fluids through a drip. You will be given pain relief as needed.
If you have a gallstone in your main bile drainage pipe, you may need to have an ERCP (endoscopic retrograde cholangiopancreatography). It is a specialised camera procedure where an instrument is used to remove the stones.
If your healthcare team decides that you need to have your gallbladder removed, this may be done while you are in hospital, especially if you are unwell. If your symptoms go away while you are in hospital, you may be put on a waiting list to have an elective operation.
Surgery to remove the gallbladder
The most common operation to remove your gallbladder is called a laparoscopic cholecystectomy. This involves removing the gallbladder using 'keyhole' surgery. You will have 3 or 4 holes made in your tummy and a telescope and light inserted to find and remove your gallbladder.
Occasionally (if the operation is more difficult than expected), the surgeon may need to switch to an open operation, which will need a bigger cut. This will leave a bigger scar and you will need a longer recovery time.
If you have your gallbladder removed, you should continue to eat well but do not need to follow a low-fat diet.
Self care to reduce the risk of gallstone attacks
If you have not had your gallbladder removed, there are things you can do to reduce the chance of having more gallstone attacks (pain or colic).
- Eat well and include plenty of vegetables, fruit and wholegrains. There is no special diet for preventing or treating gallstones, but low-fat eating may help to reduce your symptoms.
- Drink plenty of fluids. Water is best.
- Go easy on alcohol. If you drink alcohol keep within safe drinking levels.
- Avoid foods and drinks that make your symptoms worse. It may help to keep a food and symptom diary. You can then avoid your 'trigger foods'.
- Stay a healthy body weight. If you are overweight, it is best to lose weight slowly — up to 1kg per week. Losing weight quickly can increase your risk of gallstone attacks.
Low-fat eating for gallstones
Fat is a major source of fuel for our bodies and provides us with important vitamins and essential fatty acids. It is usually important as part of a healthy diet. But there may be times when you need to follow a low-fat diet. This may be because you are having trouble digesting or absorbing fat, or you have gallstones or pancreatitis.
Some foods are very high in fat. You should avoid them or only eat them occasionally. Fatty foods include:
- butter, ghee, margarine or spread, cream and all oils
- coconut cream
- mayonnaise and salad dressings made with oil
- fried foods such as fish and chips, and fatty meats such as sausages, salami and canned corned beef
- potato chips, nuts, high-fat crackers and creamy dips
- pastries, pies, cakes, biscuits and chocolate.
- Choose lean red meat or remove any visible fat from meat before you cook it.
- Take the skin off chicken after you have cooked it.
- Use low-fat cooking methods like grilling, poaching, steaming and baking instead of frying.
- Switch to lower-fat milk, either dairy or plant-based. Use this milk in cooking, on cereals and in drinks such as smoothies, milkshakes and coffee.
- Use low-fat yoghurt and reduced-fat cheese, such as edam or feta.
- Use small amounts of light or reduced-fat coconut milk instead of coconut cream.
- Choose healthier takeaway options, such as sushi or kebabs and wraps with plenty of salad.
- Avoid deep-fried food and processed meats.
- Use spray cooking oils.
- If you use spreads such as butter and margarine, use them sparingly.
If you need to follow a low-fat diet, it is important that you eat a wide variety of foods. This will help ensure you get all the nutrients your body needs to stay healthy.
Talk to your healthcare provider if:
- you are having difficulty maintaining your weight on a low-fat diet
- you are concerned you are missing out on some nutrients.
They can refer you to a dietitian.
Bread, cereals, rice, pasta, noodles
Lower-fat foods include:
- breakfast cereals with less than 10 g fat per 100 g
- plain breads including white, wholemeal, wholegrain and rye
- fruit loaf
- plain boiled pasta, low-fat noodles (vermicelli, hokkien, wheat noodles and udon) and rice
- plain sweet biscuits or low-fat savoury crackers.
High-fat foods to avoid or limit include:
- toasted cereals or muesli
- cereals containing coconut, seeds or nuts
- Turkish or focaccia bread
- croissants, donuts, muffins, pastries, cakes, muesli bars, chocolate or cream biscuits
- fried rice or instant noodles
- pasta dishes with cream or cheese sauce.
Fruit
All fresh, frozen or canned fruits are fine, except avocado and olives.
Vegetables
All vegetables are fine, as long as they are:
- steamed
- raw
- boiled
- baked without fat.
Avoid or limit:
- vegetables cooked in fat, such as fries and roast vegetables
- salads with creamy or oily dressing.
Milk and milk products
Lower-fat foods include:
- fresh, powdered or long life low-fat milks
- low-fat plant-based milk
- low-fat evaporated milk
- low-fat yoghurt, ice cream or custard
- low-fat ricotta or cottage cheese
- small amounts of reduced-fat cheese, such as Edam, Parmesan and feta.
High-fat foods to avoid or limit include:
- full-fat milk
- regular soy milk
- oat milk
- coconut cream, milk or yoghurt
- fresh cream and sour cream
- evaporated and condensed milk
- full cream and Greek yoghurt, ice cream and custard
- cream cheese and cheese spread
- full-fat cheeses.
Meat, fish, chicken, eggs, legumes, nuts and seeds
Lower-fat foods include:
- lean meat and mince, with all visible fat trimmed
- lean sandwich meats (chicken, turkey and ham)
- chicken with no skin
- eggs — poached, boiled or scrambled with no added fat
- fish and seafood – grilled, poached or baked
- canned fish in brine or spring water, 98% fat-free flavoured tuna or salmon
- legumes, such as beans, chickpeas, hummus and lentils
- tofu.
High-fat foods to avoid or limit include:
- fatty meats, such as sausages, salami, bacon, luncheon and canned corned beef
- fried chicken, chicken nuggets or chicken Kiev
- crumbed or battered fish
- oily fish such as mackerel, salmon, sardines and tuna
- canned fish in oil
- fried eggs
- fried tofu
- all nuts and nut butters.
Fats and oils
Limit extra fat to one tablespoon per day. This includes:
- butter
- margarine or spread
- cooking oils
- mayonnaise
- ghee
- lard
- oily salad dressings.